From Check-Ins To Change: Boosting Behavioral Health Outcomes With Personalized Care Journeys
Sponsored Article From

Personalized care journeys are reshaping behavioral health by focusing on individual needs instead of rigid protocols. This approach creates flexible, responsive treatment plans that evolve with each individual’s circumstances. By integrating consumer feedback, predictive insights, and continuous engagement, personalized care improves outcomes, increases consumer participation, and streamlines provider coordination.
Key Takeaways:
- What It Is: Personalized care journeys adapt treatment to each individual’s life, preferences, and progress.
- How It Works: Combines assessments, consumer input, and social factors to create dynamic care plans.
- Benefits: Better engagement, improved outcomes, and stronger care coordination.
- Core Elements: Tailored resources, matching individuals with the right providers, and ongoing measurement of progress.
- Role Of Technology: Centralized systems, mobile tools, and secure communication make personalized care scalable.
This evolution addresses the gaps in one-size-fits-all models and ensures care fits into consumers’ lives, not the other way around. By leveraging technology and continuous feedback, behavioral health providers can deliver more effective and responsive care.
The Shift To Personalized Care Journeys
The behavioral health field is undergoing a transformation as providers move away from rigid, one-size-fits-all protocols and embrace a more flexible, individualized approach. This shift reflects the shortcomings of traditional care models and the growing need for care that adapts to the unique circumstances of each person.
Problems With Standard Behavioral Health Models
Traditional behavioral health models often rely on fixed schedules and standardized protocols that don’t account for the varied needs of individuals. For example, fixed schedules can be a significant barrier for people with demanding jobs or parents juggling multiple responsibilities. These individuals may require more flexible communication and care options to fit their lives.
Another issue is that standard care is usually delivered in isolated sessions with minimal follow-up. This fragmented approach leaves many without the ongoing support they need during difficult times, creating gaps in care when it’s needed most.
How Personalized Care Responds To Life Changes
Personalized care stands out because it evolves with individuals as they navigate life’s changes. Mental health needs aren’t static—they shift with major life events. Becoming a parent, stepping into a leadership role, managing a new diagnosis, or going through family changes like divorce are just a few examples of transitions that call for tailored support.
Take new parents, for instance. They may benefit from resources on postpartum mental health and flexible appointment options to accommodate unpredictable schedules. Someone adjusting to a new job or leadership role might need stress management strategies, while those dealing with a medical diagnosis could require educational tools and coping techniques that address both emotional and practical concerns. Personalized care also considers individual differences, such as neurodiversity, by offering communication methods and interventions that align with how each person processes information.
Research Supporting Personalization
Research backs up the benefits of this approach, showing that personalized care improves engagement, symptom management, and overall treatment outcomes when care plans are tailored to an individual’s circumstances.
Technology plays a big role in making this possible. Tools like predictive analytics help providers identify patterns that suggest someone might need extra support, enabling proactive adjustments to care. Additionally, enhanced care coordination – where providers have access to shared, personalized care plans – ensures a more seamless and evolving treatment experience that meets the person’s changing needs.
Core Elements Of Personalized Care Journeys
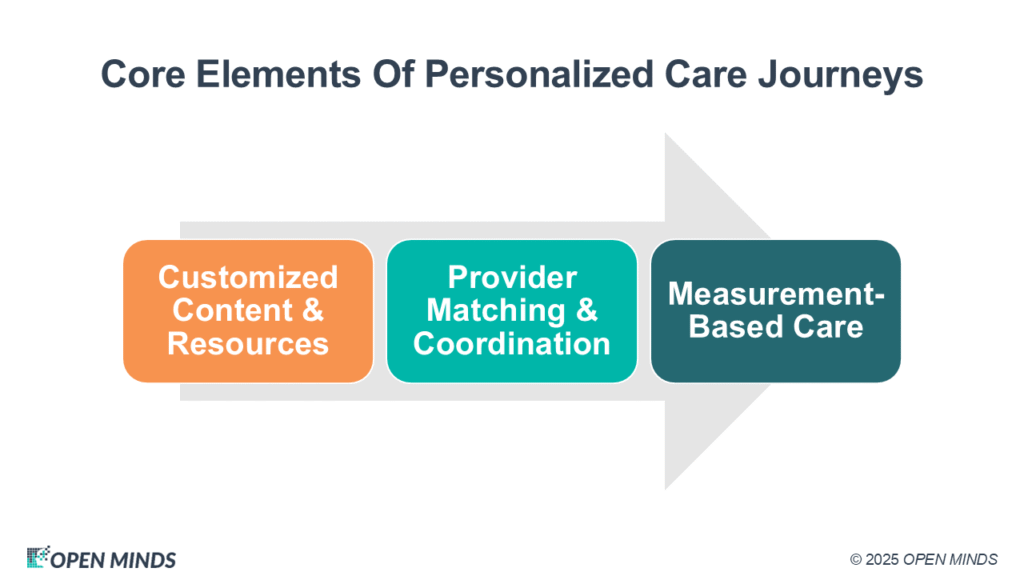
Personalized care in behavioral health revolves around three key elements that shift the focus from one-size-fits-all solutions to tailored support. These elements ensure care meets individuals where they are, addressing their unique needs and circumstances.
Customized Content & Resources
At the heart of personalized care is the delivery of timely, relevant information tailored to each person’s journey. Instead of inundating consumers with generic materials, this approach focuses on providing resources that address their specific challenges and goals.
For example, resources can be customized based on a person’s diagnosis, life stage, or personal objectives. A young adult navigating anxiety may benefit from tools that differ from those provided to someone managing a chronic condition later in life. Technology plays a crucial role here, enabling platforms to automatically deliver these tailored materials based on treatment plans, assessments, and progress markers. This not only ensures individuals receive the right support at the right time but also reduces the administrative workload for providers.
Equally important is matching individuals with the right clinician – a step that can significantly shape outcomes.
Provider Matching & Coordination
Connecting individuals with clinicians who align with their needs and preferences is a cornerstone of effective care. This goes beyond basic availability, taking into account the clinician’s specialties and therapeutic approaches. For instance, a trauma survivor may benefit most from a professional trained in trauma-informed care, while a teenager battling substance use might feel more understood by a younger clinician familiar with adolescent development.
When multiple providers are involved, care coordination becomes essential. Whether it’s a primary therapist, psychiatrist, case manager, or peer support specialist, everyone on the care team must work together seamlessly. Shared care plans accessible in real-time help ensure that all team members stay informed. For example, if a psychiatrist adjusts medication, the primary therapist can immediately incorporate this change into their sessions. Similarly, when a case manager addresses housing or employment issues, the clinical team can better understand how these changes might influence mental health progress.
This level of coordination requires clear communication protocols and reliable systems for sharing information, all while respecting privacy and confidentiality standards.
Measurement-Based Care
Personalized care thrives on regular assessments and ongoing tracking to guide decisions and fine-tune interventions. Measurement-based care involves systematically collecting data on symptoms, functioning, and goals—not just during occasional check-ins but continuously throughout treatment.
For instance, someone undergoing treatment for depression might complete weekly mood surveys, monitor sleep patterns, and assess progress toward personal milestones like improving relationships or returning to work. This data provides actionable insights. If assessments reveal worsening symptoms, the care team can adjust the treatment plan promptly instead of waiting for the next scheduled session.
Predictive analytics can also play a role, identifying patterns that indicate when an individual may need additional support or when they’re ready to transition to less intensive care. This proactive approach helps prevent crises and ensures care aligns with current needs.
Tracking progress doesn’t just benefit clinicians—it empowers individuals. Seeing tangible improvements over time and understanding which strategies work best fosters a deeper engagement in their treatment. This, in turn, equips individuals to take an active role in managing their long-term wellness.
Together, these three elements—customized resources, effective provider matching and coordination, and measurement-based care—form a dynamic framework for delivering truly personalized behavioral health treatment. Each piece works in harmony to adapt to the unique needs, preferences, and life circumstances of every individual while maintaining the clinical precision needed for successful outcomes.
How Technology Supports Personalized Care
Technology plays a crucial role in making personalized care not just possible but scalable and efficient. Without it, delivering tailored care would be a cumbersome and time-consuming process. By centralizing data and enabling mobile connectivity, technology creates a solid foundation for personalized care that meets both consumers’ and providers’ needs.
Centralizing Consumer Data With Behavioral Health Software
At the heart of personalized care is the effective management and accessibility of consumer information. Behavioral health EHR platforms bring all consumer data into one unified system, eliminating fragmented records and ensuring that care teams have all the details they need to make informed decisions.
Take ContinuumCloud’s Welligent platform, for instance. It combines scheduling, documentation, and revenue cycle management into a single, streamlined solution. This means that when a consumer updates their goals, completes an assessment, or changes medication, all relevant team members can access the updated information immediately. This level of integration simplifies workflows and enhances decision-making.
Additionally, consumer engagement platforms work hand-in-hand with EHRs to keep communication flowing. For example, ContinuumCloud’s CaredFor platform allows organizations to create online communities where individuals can receive personalized messages, access tailored resources, and communicate securely with their care teams. These platforms shift the focus from occasional check-ins to ongoing, dynamic care, ensuring consumers stay connected and supported.
Mobile Access & Secure Communication
A mobile-first approach ensures that personalized care isn’t confined to clinical settings—it becomes a part of individuals’ daily lives. With mobile access, individuals can stay engaged with their treatment plans no matter where they are.
Through mobile platforms, consumers can complete assessments, access resources, and securely communicate via messaging, push notifications, and automated reminders tailored to their individual needs. These platforms also foster peer support by enabling participation in moderated groups, mentorship programs, and educational initiatives. These community-driven interactions provide an extra layer of encouragement and support, complementing professional care.
How To Implement Personalized Care Journeys
Creating personalized care journeys requires thoughtful planning and careful execution. Jumping into implementation without preparation often leads to poor adoption and missed opportunities. To succeed, organizations need to assess their current capabilities, prepare their teams, and establish systems for ongoing improvements.
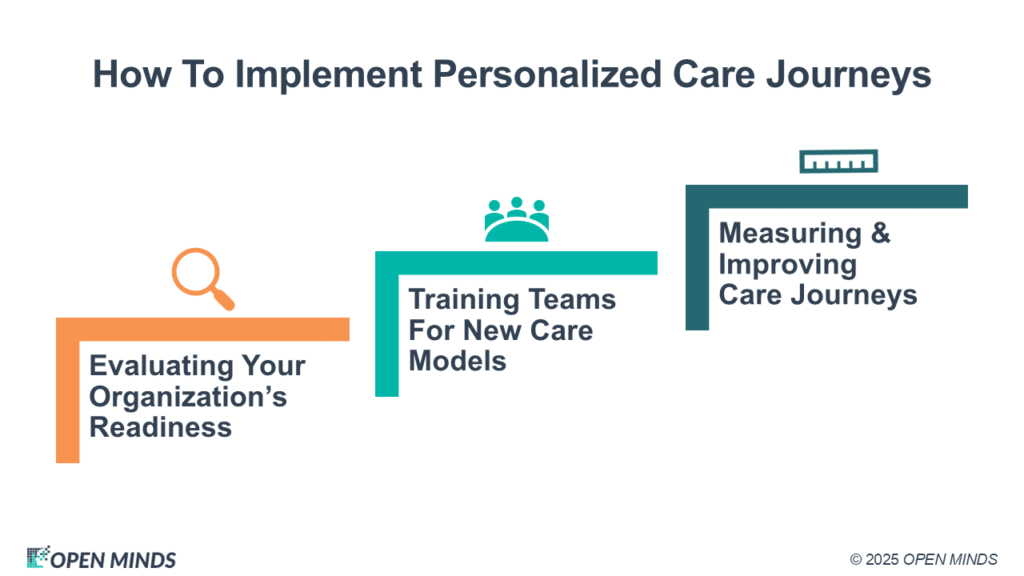
Evaluating Your Organization’s Readiness
Start by evaluating your organization’s readiness across several key areas: technology integration, staffing, consumer demographics, and financial resources. Seamless integration of systems is critical—your EHR, scheduling tools, and communication platforms must work together to provide real-time data access for providers. If these tools operate in isolation, addressing those gaps should be a priority.
Staffing is another vital factor. Personalized care requires more time upfront as providers create custom treatment plans and coordinate care across various touchpoints. Assess whether your current team can handle this increased workload, particularly during the transition when new processes are being learned.
Consumer demographics also play a role. For example, younger, tech-savvy individuals may adopt mobile engagement tools quickly, while older populations might need extra support to navigate digital platforms. Tailoring your approach to these dynamics allows for smoother implementation and realistic timelines.
Financial readiness goes beyond just purchasing software. Budget for staff training, potential dips in productivity during the transition, and ongoing support. Organizations that plan for these costs often experience fewer hurdles and better long-term results.
Once you’ve laid this groundwork, it’s time to prepare your team.
Training Teams For New Care Models
Effective training is the backbone of personalized care implementation. Clinical staff need to learn how to use new assessment tools, interpret data dashboards, and adjust treatment plans based on real-time feedback. Administrative teams must adapt to new workflows for scheduling, documentation, and consumer communication.
Specific roles require specialized training. Therapists, for instance, should understand measurement-based care and how to integrate continuous feedback into treatment planning. Case managers need skills in coordinating care across multiple providers and platforms. Front desk staff should be trained on new onboarding processes and how to assist individuals with technology-related questions.
Hands-on training can make a big difference. Use sandbox environments with realistic consumer scenarios to help teams practice the entire workflow—from initial assessments to ongoing monitoring. This approach builds confidence and familiarity with the new system.
Change management is essential during this phase. Some staff may resist new methods, especially if they’ve had success with traditional approaches. Address their concerns by demonstrating how personalized care tools can reduce administrative tasks and improve consumer outcomes. Early adopters within your team can act as champions, supporting their colleagues throughout the transition.
A phased training approach often works best. Begin with a small pilot group to test new processes and gather feedback before rolling out changes across the organization. This allows you to refine workflows and training materials based on real-world experiences.
With your team prepared, the focus shifts to measuring progress and making adjustments.
Measuring & Improving Care Journeys
To evaluate the success of personalized care, establish baseline metrics. Track indicators like consumer engagement, treatment completion rates, clinical outcomes, and provider satisfaction. These benchmarks help you measure the impact of your new approach and pinpoint areas for improvement.
Monitor consumer engagement and outcomes to identify which interventions work best for different groups. Operational metrics, such as no-show rates, length of stay, and readmission rates, can reveal process efficiencies. Financial metrics, like revenue per individual and collection rates, highlight the business value of personalized care.
Continuous improvement is key. Schedule monthly team reviews to discuss successes and areas needing adjustment. Collect structured feedback from individuals about their care experiences to refine communication templates, adjust assessment schedules, and enhance care coordination.
Technology analytics can also provide valuable insights. Many behavioral health platforms offer tools to track user engagement, feature usage, and workflow efficiency. For example, ContinuumCloud’s platforms include analytics that help organizations understand how consumers interact with their care journeys and identify opportunities for optimization.
Sharing successes is a great way to maintain momentum. Highlighting positive outcomes reinforces the value of personalized care and keeps your team motivated during the challenging implementation period.
Common Challenges In Personalization
Personalized care holds great potential, but it comes with its fair share of challenges. To truly improve behavioral health outcomes, organizations must tackle technological, operational, and compliance issues head-on. Here’s how to address some of the most pressing hurdles.
Fixing System Fragmentation
One of the toughest obstacles in personalized care is the lack of integration between different systems. Behavioral health organizations often rely on separate platforms for scheduling, documentation, billing, and consumer communication. When these systems don’t communicate, providers miss out on the full picture they need to offer individualized care.
Data silos create gaps in care delivery, making it harder to provide the seamless, informed support individuals deserve.
To solve this, start by mapping out your data flow. Document every system your organization uses, pinpointing where information gets stuck or duplicated. Look for platforms that support integrations through APIs or built-in connectors. Some organizations find it easier to switch to unified systems that handle multiple functions, reducing the need for complex connections.
Another critical step is standardizing data formats. Consistent consumer identifiers, assessment scores, and treatment codes make it easier to integrate systems and minimize errors during data transfers.
When integrating systems, focus on prioritizing connections. For example, linking your electronic health record (EHR) system with consumer engagement tools may yield faster, more impactful results than integrating less urgent systems like payroll.
Finally, remember that technology should complement—not replace—the human element in care delivery.
Balancing Automation With Human Care
While technology can simplify many aspects of personalized care, it’s essential to maintain a balance between automation and meaningful human interaction. Consumers need to feel connected to their care team, not just to automated systems.
Overusing automation can make care feel impersonal. The goal should be to use technology to enhance human-driven care, especially during critical moments in an individual’s journey.
Assign routine tasks, like appointment reminders or medication alerts, to automated systems. This frees up providers to focus on more complex cases, such as clinical decision-making, crisis management, or providing emotional support.
Customizing automated interactions can also make a big difference. For instance, instead of sending generic motivational messages, tailor communications to reflect an individual’s progress, preferences, or treatment goals. This keeps the efficiency of automation while preserving a personal touch.
Training staff to work alongside automated tools is equally important. Providers need to know when to intervene. For example, if an automated check-in flags concerning symptoms or missed appointments, a human response should follow immediately.
Lastly, educating consumers about these technologies fosters trust. When individuals understand how their data is being used to improve their care, they’re more likely to engage with both the tools and their care team.
Data Security & Compliance
Personalized care involves collecting, storing, and sharing more consumer information than traditional models, which increases the risk of security breaches and compliance issues. Protecting consumer privacy while staying compliant with regulations like HIPAA is a top priority.
With personalized care systems, HIPAA compliance becomes increasingly complex. Every platform, integration, and data-sharing process must meet strict privacy standards. This includes mobile apps, patient portals, and communication tools, all of which require proper safeguards and business associate agreements.
Cloud-based platforms and third-party vendors add another layer of complexity. Every vendor in your technology stack must demonstrate compliance, and you’ll need clear documentation of how individuals’ data flows between systems. Regular audits and strong encryption are essential to prevent data breaches.
Access controls are also critical. Different team members require access to different types of consumer information, and these permissions should be regularly reviewed and updated. For example, a case manager might need access to treatment plans, while a billing specialist only needs financial details.
Encryption is non-negotiable. Protect data at every stage—whether it’s in transit, stored in databases, or shared between systems. Maintaining encryption across multiple platforms can be challenging, but it’s vital for safeguarding consumer information.
Finally, have a clear breach response plan in place. Your organization should establish robust policies and procedures to address potential security incidents quickly and effectively.
Consumer consent management is another key area. Make sure individuals can easily give or modify their consent for data sharing. This not only builds trust but also ensures coordinated care when sharing information with other providers, family members, or community resources.
Conclusion
The transition from routine check-ins to truly personalized care journeys is reshaping behavioral health by focusing on each individual’s unique circumstances. This approach moves away from rigid, one-size-fits-all models, creating care pathways that align with individual preferences and treatment goals.
In this guide, we’ve highlighted the key elements driving these personalized journeys: tailored content, provider matching, and measurement-based care. At the heart of these advancements lies technology—behavioral health software, mobile tools, and secure communication platforms—that fosters a supportive and engaging environment for consumers throughout their treatment.
Yet, achieving success in this new model takes more than just adopting new tools. Organizations must tackle challenges like system fragmentation, strike a balance between automation and human connection, and uphold strict data security standards. While these hurdles are real, the potential rewards—better consumer outcomes, higher engagement, and more efficient care—underscore the importance of this shift. This evolution signals a dynamic and responsive future for behavioral health.
The Future Of Behavioral Health Care
Behavioral health is adapting to meet the diverse, ever-changing needs of individuals. Personalized care journeys are at the forefront of this evolution, offering treatments that mold to the individual rather than forcing individuals to conform to rigid protocols.
This approach recognizes that recovery isn’t a straight path. Effective care must account for life’s ups and downs, setbacks, and the unique pace at which each individual progresses. Organizations embracing this model are better positioned to deliver improved outcomes while fostering deeper connections with the communities they serve.
As these technologies continue to develop, the gap between consumer needs and provider organization capabilities will shrink, paving the way for a more consumer-centered approach to care.
Next Steps
For organizations ready to adopt personalized care journeys, success begins with thoughtful planning and smart technology integration. Start by evaluating your current systems to break down data silos and improve coordination.
Consider investing in a comprehensive behavioral health platform to simplify the shift to personalized care while ensuring compliance and data security.
Equip your team with the skills to use technology effectively, ensuring it complements—rather than replaces—clinical expertise and empathy. Develop workflows that enhance human connection while leveraging the efficiency of digital tools.
To build momentum, launch targeted pilot programs to test and refine your personalized care approach. Use these smaller-scale initiatives to gather data, measure outcomes, and fine-tune processes before expanding organization-wide.
FAQs
How does personalized care enhance consumer engagement and improve outcomes in behavioral health?
Personalized care takes consumer engagement to the next level by addressing the specific needs, preferences, and circumstances of each individual. This approach doesn’t just treat symptoms—it digs deeper to uncover the underlying causes of mental health challenges, leading to more effective and lasting results.
When treatment plans are tailored to the individual, consumers tend to feel more involved and empowered in their care. This sense of ownership strengthens the collaboration between consumers and providers, making it easier to stick to treatment plans and achieve better outcomes. Studies repeatedly highlight that customized interventions deliver better results compared to generic, one-size-fits-all methods in behavioral health settings.
How does technology support personalized care journeys while ensuring data security and compliance?
Technology plays a key role in crafting personalized care journeys, giving providers the tools to create treatment plans tailored to each individual while encouraging stronger collaboration between consumers and provider organizations. With advanced solutions like behavioral health software and engagement platforms, providers can develop customized tasks, resources, and surveys that guide individuals through care experiences designed specifically for their needs. This approach not only addresses individual challenges but also aims to improve outcomes, particularly in behavioral health and substance use treatment.
Equally important, these technologies come equipped with strong data security and compliance features to safeguard sensitive consumer information. By adhering to healthcare regulations such as HIPAA, they ensure that care remains personalized without compromising consumer privacy or trust.
What are the key steps organizations can take to implement personalized care journeys and address common challenges?
To put personalized care journeys into action, organizations should focus on crafting care plans that genuinely reflect each individual’s specific needs, preferences, and goals. This means encouraging open collaboration between individuals and healthcare provider organizations, giving individuals an active role in their treatment decisions, and frequently revisiting and adjusting care plans to ensure they stay on track.
Another key element is empowering individuals with education and tools for self-management. Offering resources like health and wellness coaching, connecting individuals to local support networks, and addressing broader factors like social determinants of health can help create a more well-rounded approach to care. By prioritizing these efforts, organizations can boost consumer outcomes and foster deeper engagement.

