Technology-Enabled Financial Health: A Strategic Framework
In today’s health care environment, the effectiveness of a provider organization’s technology infrastructure is not measured by the value of individual platforms alone but by how thoroughly the array of systems integrates to enhance financial, clinical, and operational performance. Fragmented systems that silo information fail to equip leadership teams with the visibility into data, metrics, and analytics needed to develop the insights that drive strategic decision-making. Executives leading provider organizations require cohesive, integrated technology tools that together form an information ecosystem.
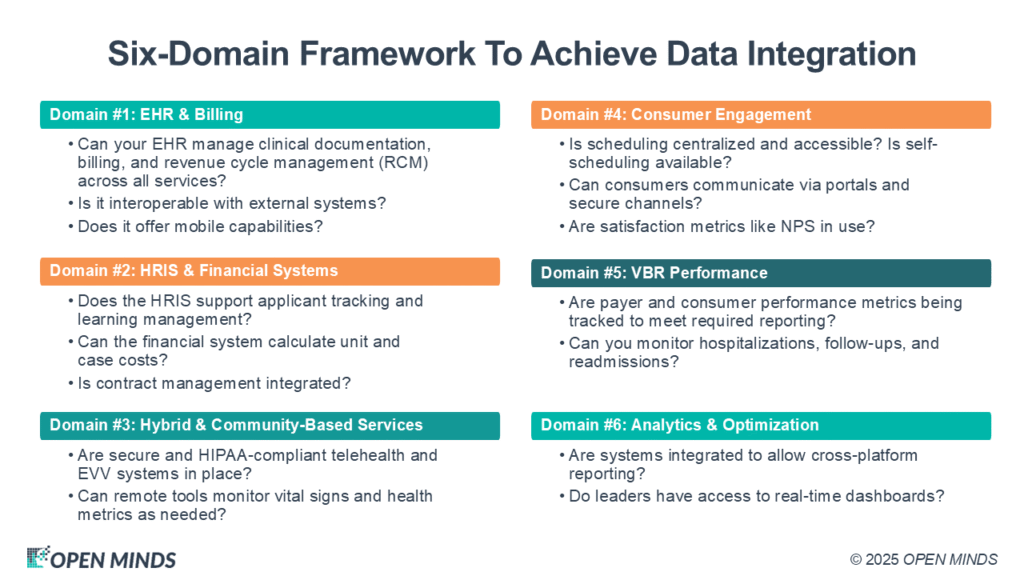
To help assess, build, and optimize a technology platform that can support both current operations and long-term strategic objectives, executive teams can use this comprehensive six-domain framework to achieve necessary data integration and visibility:
Domain #1: A Comprehensive EHR
To achieve and maintain financial strength and monitor metrics for signs of trouble, a fully functional electronic health record (EHR) serves as the core of a technology-enabled delivery model, not just a repository for clinical notes and billing functions. To be fully functioning, it must deliver these seven elements:
- Record consumer demographic and clinical data across all service lines and make it easy to update when that information changes.
- Document referrals and track and trend outcomes.
- Track quality, performance, and compliance metrics.
- Support standard clinical features such as electronic prescribing of various classes of medications, including controlled substances (EPCS); sending and receiving lab orders and lab results; documenting electronic medication administration (eMAR); medication reconciliation; and prescription drug monitoring programs (PDMP) compliance.
- Enable multidisciplinary treatment plans with clinical documentation and claims tools that include primary care services.
- Enable mobile access so care team members can meet consumers where they are. Provide clinical decision support tools that align with payer requirements and evidence-based care pathways for quality improvement and compliance. Support reimbursement under various payment models, from fee-for-service to value-based reimbursement (VBR) and contracts that include wraparound services.
- Support secure two-way messaging to enable communication between consumers and care teams.
Ultimately, EHR evaluation must be based on its strengths in supporting care teams and in its capabilities in enabling all teams to collect, track, and analyze the financial and operational data that derives from completed appointments. Supporting whole person care means both offering cross-disciplinary documentation tools and enabling complex billing models. The financial health of an organization depends on executive teams having access to services offered, services completed, productivity, and all the operational data that can be extracted from programs and services, from productivity to costs and revenues.
Domain #2: Human Resource & Financial Systems
Human resource and financial systems (HRIS) and financial/general ledger systems form the administrative backbone of an organization and are critical for managing both the financials at an organization and an organization’s biggest expense—staffing. These tools must go beyond basic functions and provide elevated capabilities in two areas:
- The HRIS should support applicant tracking, time and attendance, employee self-service, and learning management. It must also enable employee development plans and appraisals in support of performance management and performance improvement.
- The financial system must facilitate budgeting, payroll, accounts payable, and asset tracking. It should also support cost-of-service reporting and contract management across all payment models, allowing chief financial officers (CFOs) to know “where every dollar goes” and then make adjustments in the service of a better revenue/cost balance.
To support contracts of all kinds—but especially VBR, alternate payment models, and preferred provider status—these systems must integrate with EHRs and other systems, such as call centers—to produce real-time insights into service costs and operational efficiency.
Domain #3: Community & Virtual Care Platforms
The health care field has seen virtual care—including telehealth, online, hybrid, and tech-enabled community-based services—become essential, but these platforms must be more than simple virtual appointments. The modern service delivery platform must:
- Integrate secure and HIPAA-compliant telehealth capabilities into the EHR.
- Enable mobile use by field staff, including EHRs, to meet people where they are. Incorporate electronic visit verification (EVV) that integrates into the EHR.
- Support smart home monitoring and secure, multi-format communication (text, email, video) that integrates into the EHR.
- Offer route optimization tools for in-community care delivery that integrate into the EHR and the EVV solution.
On the one hand, this domain ensures flexibility and responsiveness to consumer needs, especially for populations with complex care requirements. The result can be better services, better care, and better outcomes. On the other hand, it also supports the real-time collection of accurate data and the ability to manage the performance needed to protect a provider organization’s financial health.
Domain #4: Customer Experience & Engagement Tools
As consumer expectations rise, specialty providers must treat consumer experience as a strategic priority that can protect both service use and the outcomes of those services—the right tools can improve access, satisfaction, and outcomes—all of which can be used to enhance and protect financial strength. Key capabilities include:
- Centralized, 24/7 access to care.
- User-friendly websites with online self-scheduling.
- Secure two-way messaging and portals for communication, billing, health record access, and the capability for consumers to complete forms in advance of appointments.
- Self-directed wellness applications.
- Net promoter scoring is integrated into service workflows.
- Automated appointment reminders and follow-ups as an aspect of outreach to drive better outcomes and enhance productivity by enabling better management of provider schedules and productivity.
Organizations must assess current assets and identify technology gaps to build a seamless, high-touch digital front door as consumer expectations increasingly demand one.
Domain #5: Value-Based Reimbursement Performance Tools
As reimbursement models shift, technology must support the rigorous demands of value-based care. Executive teams should prioritize tools that:
- Integrate evidence-based practices into clinical workflows to drive clinical outcomes, enhance quality, and meet and exceed compliance requirements.
- Track access, engagement, and other metrics that can be part of payer contracts, grant requirements, and compliance requirements (e.g., HEDIS, CCBHC requirements).
- Report on social determinants of health (SDOH), health-related social needs (HRSNs), and other risk factors.
When these requirements cannot be met within the EHR, integration with third-party tools can be required to gain analytics dashboards, performance monitoring software, and intelligent reporting systems that are vital to success in gaining a preferred provider relationship with payers and for high performance under VBR models.
Domain #6: Integrated Analytics & Optimization
This final domain is the connective tissue between data and strategic decision-making. Advanced analytics platforms that can be available within EHRs or can be integrated as third-party tools enable organizations to:
- Aggregate data across systems.
- Produce real-time dashboards for leadership and staff.
- Track key performance indicators tied to strategic objectives.
Business intelligence (BI) tools that start with data collection and reporting can evolve into population health management engines—segmentation, predictive analytics, and intervention strategies all stem from this foundation.
The Path Forward: Strategic Assessment
How can organizations advance their tech platforms? The process begins with an internal assessment of core functionality and alignment with strategic priorities. On the path to an integrated system that can support sustainable financial health, consider these 18 essential technology capabilities across the six domains presented above:
EHR & Billing
- Can your EHR manage clinical documentation, billing, and revenue cycle management (RCM) across all services?
- Is it interoperable with external systems?
- Does it offer mobile capabilities?
HRIS & Financial Systems
- Does the HRIS support applicant tracking and learning management?
- Can the financial system calculate unit and case costs?
- Is contract management integrated?
Hybrid & Community-Based Services
- Are secure and HIPAA-compliant telehealth and EVV systems in place?
- Can remote tools monitor vital signs and health metrics as needed?
Consumer Engagement
- Is scheduling centralized and accessible? Is self-scheduling available?
- Can consumers communicate via portals and secure channels?
- Are satisfaction metrics like NPS in use?
VBR Performance
- Are payer and consumer performance metrics being tracked to meet required reporting?
- Can you monitor hospitalizations, follow-ups, and readmissions?
Analytics & Optimization
- Are systems integrated to allow cross-platform reporting?
- Do leaders have access to real-time dashboards?
- Is data literacy promoted throughout the organization?
This kind of audit serves as both a readiness check and a roadmap. Areas of deficiency—particularly in foundational systems like EHRs and financial platforms—should be prioritized for immediate investment.
Strategic Technology Planning: From Audit To Action
Beyond operational readiness, technology strategy must align with the organization’s broader vision. Executive teams should crosswalk strategic goals with required tech capabilities. Are you expanding service lines? Pursuing new VBR contracts? Launching population health initiatives? Which elements of an integrated system can the organization afford now, soon, or in the long run?
Each goal introduces new technology requirements. For example:
- Expanding access may necessitate investment in consumer portals or customer relationship management (CRM) tools.
- Entering new VBR arrangements may require enhanced analytics for real-time performance tracking.
- Scaling community-based care may demand route optimization, EVV, and remote monitoring.
Building a technology roadmap requires interdisciplinary input. Chief information officers (CIOs), chief technology officers (CTOs), and chief financial officers (CFOs) will play the critical roles in identifying what functionalities and what returns on investment are needed. Just remember that strategy cannot rest solely with a single leader or team. Every executive must engage with the imperative to both integrate the technology system and put it into management practice.
Leading In The Era Of Digital Health
The future of specialty health care is being shaped by organizations that treat technology not just as the infrastructure supporting a strategy, but as a strategy unto itself. Or, as the media theorist Marshall McLuhan put it, “The medium is the message.”
For provider organization executives who need to “manage by the numbers,” this means that the way data and information are collected, analyzed, and conveyed will have as strong an impact as the actual content itself. (For more on the importance of information literacy, check out this issue’s article, Diagnosing Financial Health: Metrics Meet Information Literacy). Technology must empower better decisions, enable scalable service models, and position the organization for financial sustainability. That kind of technological maturity can deliver a competitive advantage, but only if teams continuously evaluate where they are on the journey and what investments are needed to take the next step.